Prior Authorization: Common Challenges and Exactly How to Get rid of T…
페이지 정보
작성자 Estela 작성일25-08-01 16:48본문
Picture this: you have actually simply covered up an examination with a client, recommended a life-altering drug or an essential diagnostic test, and feel great that they get on the course to healing. Then, a curveball strikes-- the dreaded phone call from the insurance business: "We need prior permission for this treatment." Unexpectedly, whatever pertains to a shrilling stop.
Noise acquainted? If you're a medical care professional, possibilities are you've handled the irritating and commonly time-consuming world of prior authorization (PA). This process, while necessary for managing medical care costs, can seem like a limitless maze of documentation, call, and hold-ups that stand up client treatment.
But here's the excellent news: You don't need to face these challenges alone. In this article, we'll check out the usual difficulties in the PA procedure and provide sensible suggestions on how to conquer them. Whether you're a medical professional, nurse, or workplace manager, these techniques can help you browse the labyrinth extra effectively-- so you can concentrate on what really matters: your individuals.
1. Obstacle # 1: Lengthy Authorization Times
The Issue: Among one of the most usual frustrations with prior consent is the wait. While you and your individual rest on pins and needles, the insurance firm takes its wonderful time making a decision whether or not to accept a therapy. It can take anywhere from numerous days to weeks, which not only delays care yet additionally raises client anxiousness.
The Remedy: Beginning early. The quicker you send a prior permission request, the much less likely it is to disrupt your patient's therapy routine. Ideally, you must send demands immediately-- prior to the individual leaves the office. If you're intending a surgery or prescribing a specialized medicine, make certain your workplace team recognizes the requirements from the start.
Pro Tip: Usage digital prior consent (ePA) devices to automate submissions. Solutions like CoverMyMeds or your EHR's incorporated attribute permit you to send demands directly to insurers, simplifying the process and lowering the chances of delays created by missing documentation.
2. Difficulty # 2: Constant Rejections
The Issue: It's the moment you have actually been dreading: your previous consent demand gets denied. Denials are frustrating because they're commonly based on "insufficient paperwork," "medical need," or "different therapies readily available," also when you and your person understand that the recommended therapy is specifically what's required.
The Remedy: Charm, charm, charm! When a PA request is rejected, do not approve it as the last word. Most insurance policy strategies allow for a charm procedure, and several rejections are rescinded upon evaluation. The trick is to give comprehensive, well-documented evidence to support your instance. Ensure your demand consists of specific information regarding why the therapy or medicine is medically needed, and if appropriate, offer alternatives that were thought about.
Pro Idea: Keep all documents arranged and conveniently obtainable. A layout for appeal letters can conserve you time and ensure you're regularly offering the best supporting details for each and every case. Don't neglect to include your individual in the process-- they can often add effective personal context that reinforces your appeal.
3. Obstacle # 3: Complex Insurance Policy Demands
The Problem: Each insurance firm has its own collection of regulations, kinds, and treatments for submitting previous authorization demands. This inconsistency can lead to confusion, errors, and a considerable amount of lost time as you determine how to browse each insurance firm's unique system.
The Solution: Get acquainted with the major insurance firms your technique deals with. If you frequently treat individuals with certain insurance policy plans, learn the ins and outs of those service providers' prior consent guidelines. Make a list for typical requirements-- some insurers call for various documentation for the exact same procedure, and having a fast referral guide will certainly save you effort and time.
Pro Pointer: Create a cheat sheet of common prior consent requirements for your workplace personnel. This can include points like types to use, preferred approaches of submission (fax, portal, phone), and any kind of particular requirements insurance companies generally try to find in approvals.
4. Difficulty # 4: Absence of Communication Between Providers and Insurers
The Problem: The previous permission procedure commonly feels like a game of telephone-- your office sends a demand, waits weeks for a response, and after that you're left asking yourself whether the demand was even received or where it's at in the approval procedure. Meanwhile, your person is left waiting, unclear of what's taking place.
When submitting a prior permission demand, make certain to comply with up frequently with the insurance firm to confirm they received it and ask for updates. Some insurance providers even have devoted teams that you can get to out to straight.
Pro Idea: Usage automated monitoring devices to keep tabs on your demands. Many insurer currently provide sites where you can inspect the standing of your request in real time. If you don't have accessibility to this, take into consideration setting up reminders in your EHR system to follow up periodically.
5. Obstacle # 5: Management Burden on Office Team
The Trouble: Handling prior permission requests can take a substantial toll on your office personnel. Taking care of the documentation, telephone call, and follow-ups can be frustrating, bring about exhaustion and inefficiencies.
The Remedy: Delegate and digitize. When possible, assign 1 or 2 team participants to be your workplace's professionals. This will certainly simplify the procedure and make certain that your staff can focus on their key obligations without obtaining slowed down by administrative jobs. In addition, purchase electronic PA systems to minimize hand-operated information entrance and simplify the approval process.
Pro Tip: Contract out monitoring to a third-party service if the volume is expensive for your group. These services can handle the bulk of the management work, leaving your workplace totally free to concentrate on client treatment.
6. Difficulty # 6: Irritated Clients
The Issue: Nothing is extra aggravating for a client than being told their therapy is delayed due to a prior permission process. The stress and anxiety of waiting on approval, integrated with the uncertainty of whether they'll be able to get the treatment they require, can make an already tight spot worse.
The Remedy: Set clear expectations. When you're very first preparing a therapy strategy, google_vignette be ahead of time with your patients regarding the opportunity of hold-ups as a result of prior permission. Keep them in the loop and, if feasible, supply normal updates on the status of their demand. Being clear and aggressive can decrease anxiety and construct trust with your patients.
Pro Pointer: Usage automated interaction tools to send out clients real-time updates on the condition of their treatment. Whether it's via an on the internet site or sms message, individuals will appreciate the transparency and really feel more in control of their care.
Final Thought: Prior Authorization Does Not Have to Be an Obstacle
By starting early, getting familiar with insurance policy requirements, utilizing technology to streamline the process, and keeping clear interaction with both clients and insurers, you can overcome the common obstacles that come with PA
. Think about training your personnel, utilizing ePA tools, and producing a clear communication strategy for both clients and insurance firms. With a little preparation and an aggressive state of mind, you can turn previous authorization from a stumbling block right into a smooth step in your treatment distribution process.
After all, your people are entitled to the best care-- and that begins with making the procedure benefit you, not versus you.
Whether you're a medical professional, nurse, or workplace manager, these methods can help you navigate the PA maze more efficiently-- so you can concentrate on what actually matters: your clients.
The earlier you submit a prior authorization demand, the less most likely it is to interfere with your client's treatment timetable. Ideally, you must submit requests as soon as possible-- before the individual leaves the office. If you consistently deal with individuals with certain insurance policy plans, learn the ins and outs of those service providers' previous permission standards. When you're initial planning a treatment strategy, be ahead of time with your people about the possibility of delays due to previous permission.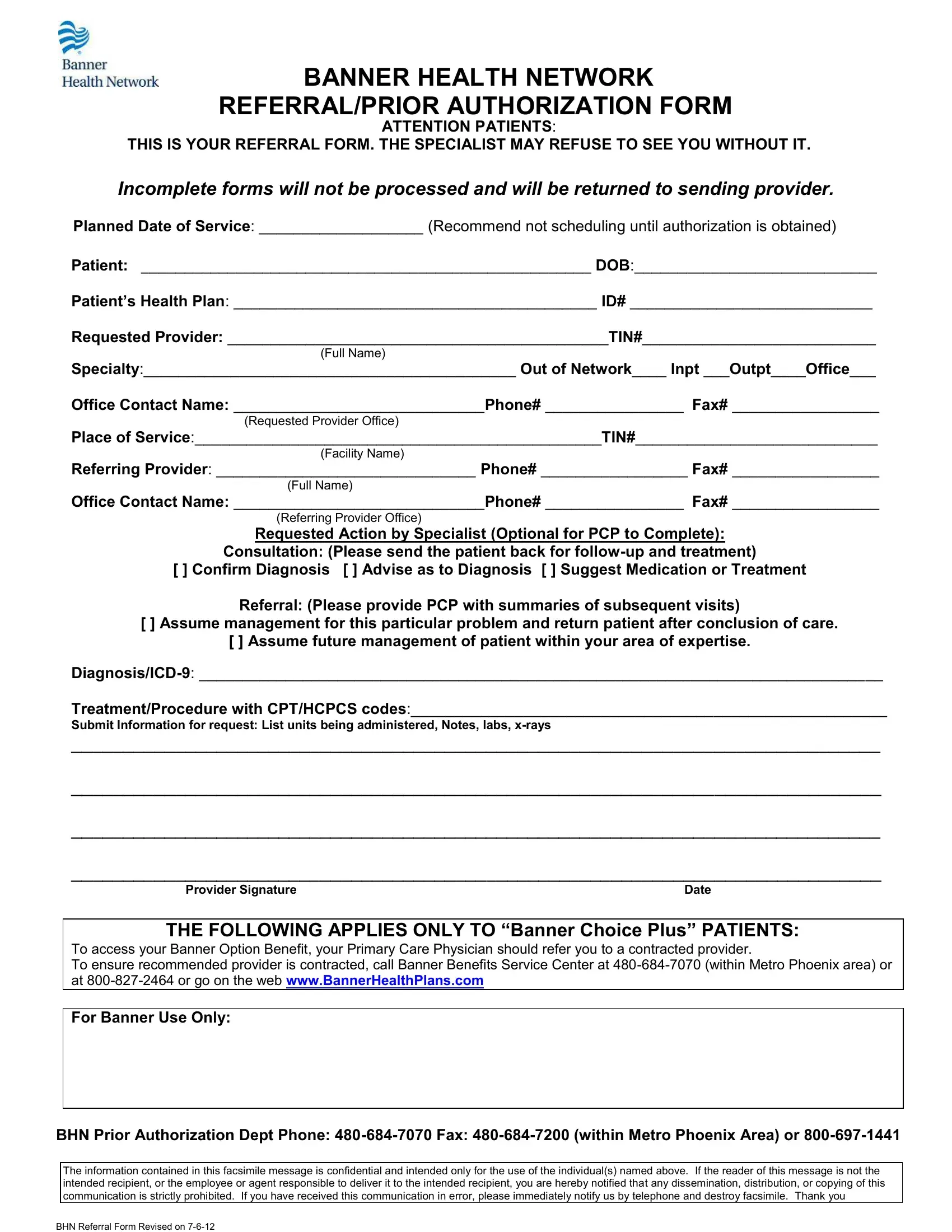
Noise acquainted? If you're a medical care professional, possibilities are you've handled the irritating and commonly time-consuming world of prior authorization (PA). This process, while necessary for managing medical care costs, can seem like a limitless maze of documentation, call, and hold-ups that stand up client treatment.
But here's the excellent news: You don't need to face these challenges alone. In this article, we'll check out the usual difficulties in the PA procedure and provide sensible suggestions on how to conquer them. Whether you're a medical professional, nurse, or workplace manager, these techniques can help you browse the labyrinth extra effectively-- so you can concentrate on what really matters: your individuals.
1. Obstacle # 1: Lengthy Authorization Times
The Issue: Among one of the most usual frustrations with prior consent is the wait. While you and your individual rest on pins and needles, the insurance firm takes its wonderful time making a decision whether or not to accept a therapy. It can take anywhere from numerous days to weeks, which not only delays care yet additionally raises client anxiousness.
The Remedy: Beginning early. The quicker you send a prior permission request, the much less likely it is to disrupt your patient's therapy routine. Ideally, you must send demands immediately-- prior to the individual leaves the office. If you're intending a surgery or prescribing a specialized medicine, make certain your workplace team recognizes the requirements from the start.
Pro Tip: Usage digital prior consent (ePA) devices to automate submissions. Solutions like CoverMyMeds or your EHR's incorporated attribute permit you to send demands directly to insurers, simplifying the process and lowering the chances of delays created by missing documentation.
2. Difficulty # 2: Constant Rejections
The Issue: It's the moment you have actually been dreading: your previous consent demand gets denied. Denials are frustrating because they're commonly based on "insufficient paperwork," "medical need," or "different therapies readily available," also when you and your person understand that the recommended therapy is specifically what's required.
The Remedy: Charm, charm, charm! When a PA request is rejected, do not approve it as the last word. Most insurance policy strategies allow for a charm procedure, and several rejections are rescinded upon evaluation. The trick is to give comprehensive, well-documented evidence to support your instance. Ensure your demand consists of specific information regarding why the therapy or medicine is medically needed, and if appropriate, offer alternatives that were thought about.
Pro Idea: Keep all documents arranged and conveniently obtainable. A layout for appeal letters can conserve you time and ensure you're regularly offering the best supporting details for each and every case. Don't neglect to include your individual in the process-- they can often add effective personal context that reinforces your appeal.
3. Obstacle # 3: Complex Insurance Policy Demands
The Problem: Each insurance firm has its own collection of regulations, kinds, and treatments for submitting previous authorization demands. This inconsistency can lead to confusion, errors, and a considerable amount of lost time as you determine how to browse each insurance firm's unique system.
The Solution: Get acquainted with the major insurance firms your technique deals with. If you frequently treat individuals with certain insurance policy plans, learn the ins and outs of those service providers' prior consent guidelines. Make a list for typical requirements-- some insurers call for various documentation for the exact same procedure, and having a fast referral guide will certainly save you effort and time.
Pro Pointer: Create a cheat sheet of common prior consent requirements for your workplace personnel. This can include points like types to use, preferred approaches of submission (fax, portal, phone), and any kind of particular requirements insurance companies generally try to find in approvals.
4. Difficulty # 4: Absence of Communication Between Providers and Insurers
The Problem: The previous permission procedure commonly feels like a game of telephone-- your office sends a demand, waits weeks for a response, and after that you're left asking yourself whether the demand was even received or where it's at in the approval procedure. Meanwhile, your person is left waiting, unclear of what's taking place.
When submitting a prior permission demand, make certain to comply with up frequently with the insurance firm to confirm they received it and ask for updates. Some insurance providers even have devoted teams that you can get to out to straight.
Pro Idea: Usage automated monitoring devices to keep tabs on your demands. Many insurer currently provide sites where you can inspect the standing of your request in real time. If you don't have accessibility to this, take into consideration setting up reminders in your EHR system to follow up periodically.
5. Obstacle # 5: Management Burden on Office Team
The Trouble: Handling prior permission requests can take a substantial toll on your office personnel. Taking care of the documentation, telephone call, and follow-ups can be frustrating, bring about exhaustion and inefficiencies.
The Remedy: Delegate and digitize. When possible, assign 1 or 2 team participants to be your workplace's professionals. This will certainly simplify the procedure and make certain that your staff can focus on their key obligations without obtaining slowed down by administrative jobs. In addition, purchase electronic PA systems to minimize hand-operated information entrance and simplify the approval process.
Pro Tip: Contract out monitoring to a third-party service if the volume is expensive for your group. These services can handle the bulk of the management work, leaving your workplace totally free to concentrate on client treatment.
6. Difficulty # 6: Irritated Clients
The Issue: Nothing is extra aggravating for a client than being told their therapy is delayed due to a prior permission process. The stress and anxiety of waiting on approval, integrated with the uncertainty of whether they'll be able to get the treatment they require, can make an already tight spot worse.
The Remedy: Set clear expectations. When you're very first preparing a therapy strategy, google_vignette be ahead of time with your patients regarding the opportunity of hold-ups as a result of prior permission. Keep them in the loop and, if feasible, supply normal updates on the status of their demand. Being clear and aggressive can decrease anxiety and construct trust with your patients.
Pro Pointer: Usage automated interaction tools to send out clients real-time updates on the condition of their treatment. Whether it's via an on the internet site or sms message, individuals will appreciate the transparency and really feel more in control of their care.
Final Thought: Prior Authorization Does Not Have to Be an Obstacle
By starting early, getting familiar with insurance policy requirements, utilizing technology to streamline the process, and keeping clear interaction with both clients and insurers, you can overcome the common obstacles that come with PA
. Think about training your personnel, utilizing ePA tools, and producing a clear communication strategy for both clients and insurance firms. With a little preparation and an aggressive state of mind, you can turn previous authorization from a stumbling block right into a smooth step in your treatment distribution process.
After all, your people are entitled to the best care-- and that begins with making the procedure benefit you, not versus you.
Whether you're a medical professional, nurse, or workplace manager, these methods can help you navigate the PA maze more efficiently-- so you can concentrate on what actually matters: your clients.
The earlier you submit a prior authorization demand, the less most likely it is to interfere with your client's treatment timetable. Ideally, you must submit requests as soon as possible-- before the individual leaves the office. If you consistently deal with individuals with certain insurance policy plans, learn the ins and outs of those service providers' previous permission standards. When you're initial planning a treatment strategy, be ahead of time with your people about the possibility of delays due to previous permission.
댓글목록
등록된 댓글이 없습니다.